Most people think “black spot = cavity,” but tooth decay usually starts as chalky white areas (early demineralization), then progresses to softened brown/black zones, and finally opens into pits or holes. Spotting these visual cues early means simpler, cheaper care that preserves natural tooth.
TL;DR — What does tooth decay look like?
Chalky, matte white patches → brown/black soft areas → visible pits/holes. Between-teeth disease is often invisible in a mirror and first appears as a triangular shadow on bitewing X-rays.
Why appearance matters (color ≠ severity)
Tooth color alone misleads. Texture (hard vs. soft), location, and whether food traps or sensitivity occurs tell you more. Hard, glossy grooves may just be stain; soft, rough surfaces strongly suggest decay.
By stage: how it looks in real life
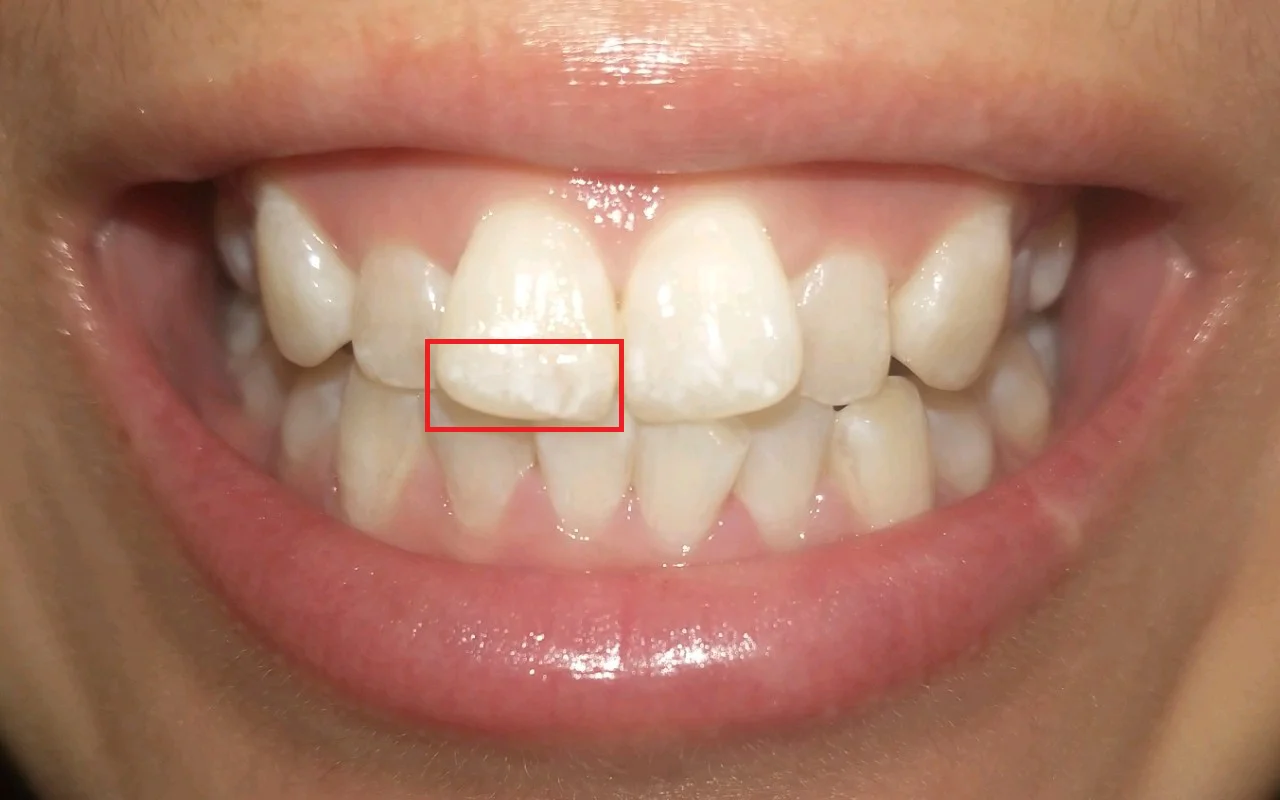
Early white-spot lesions (reversible)
Look: Chalky, matte white near gumlines/fissures; less glossy than nearby enamel.
Clues: No pain; more obvious when the tooth is dry.
Do: 1000–1500 ppm fluoride toothpaste twice daily; reduce sugary snack frequency; see a dentist for fluoride varnish or resin infiltration.
Stained & softened enamel/dentin (no obvious hole)
Look: Light-brown → dark-brown/black specks or lines; the key is softness, not color.
Clues: Persistent food trapping; sweet/cold sensitivity.
Do: Book a visit soon for micro-invasive cleaning and a small filling to halt tooth decay before the surface breaks.
Cavitation (a visible hole)
Look: A pit/hole with undermined, crumbly edges; debris often packs inside.
Clues: Sweet/cold pain or bite tenderness; late cases can cause night pain.
Do: Composite fillings or inlays/onlays; deep lesions may need a root canal.
By location: common patterns you can recognize
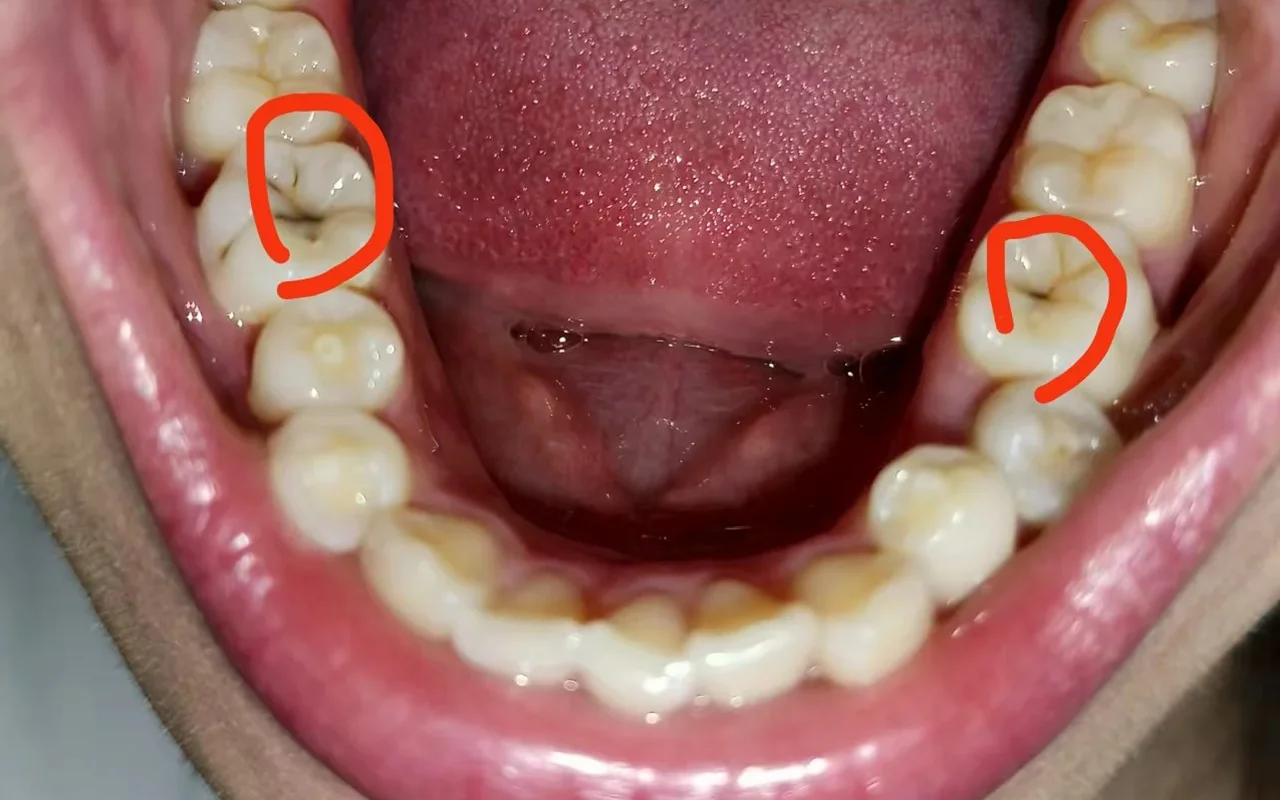
Chewing surfaces (fissure/occlusal decay)
Tiny dark dots/lines in grooves. Color ≠ severity—softness and extent (plus X-rays) decide.
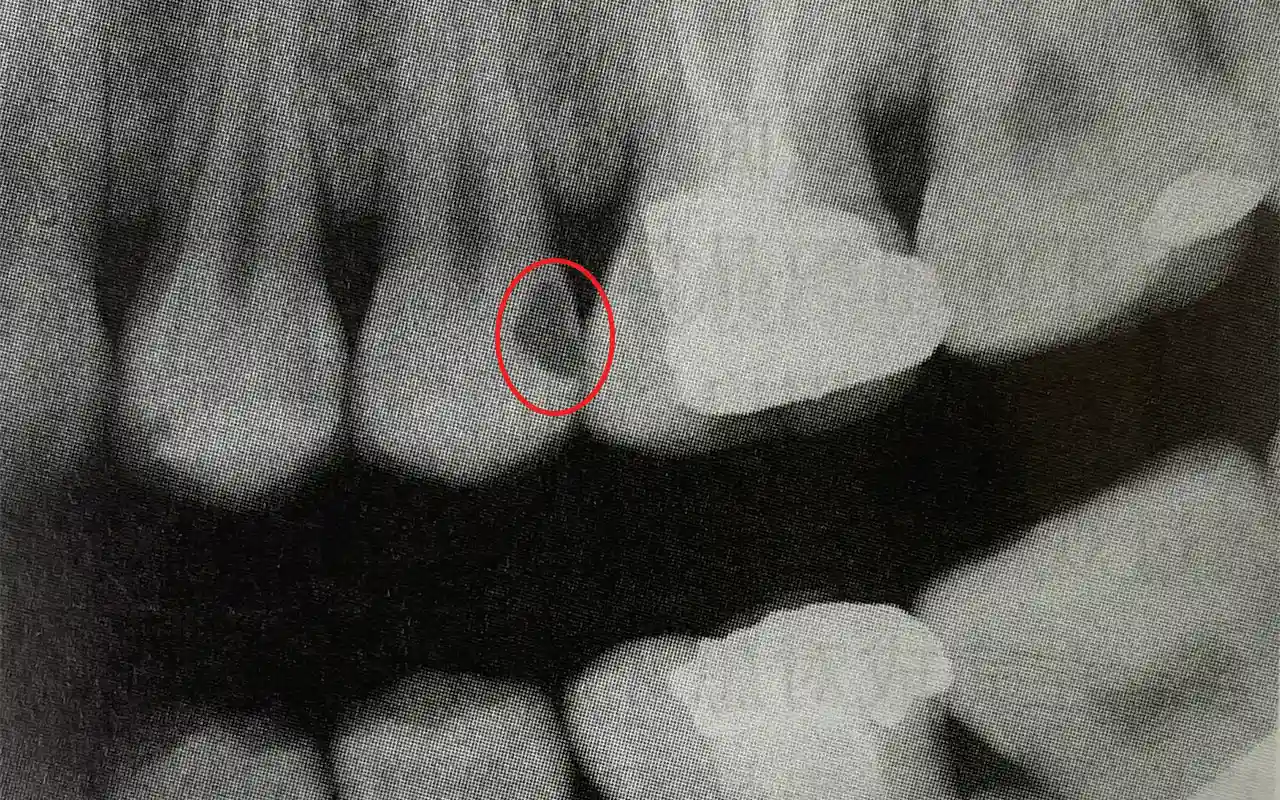
Between teeth (interproximal tooth decay)
Often invisible in the mirror. Home hints: floss snags or frays, and food routinely packs.
Bitewing X-ray: a triangular radiolucency beneath the contact point.
Near the gumline & on roots (cervical/root caries)
Yellow-brown, soft bands where gums have receded. Distinguish from wedge lesions/abrasion (hard, glossy, sharp-edged).

In young children (early childhood caries)
Starts as white bands by the gumline on upper front teeth → turns yellow-brown and chips quickly. Linked to frequent sugars or bedtime milk/juice without cleaning.

Look-alikes that aren’t decay
Tea/coffee/iron stains: dark but hard and smooth; polishable.
Black line stain (kids): cleanable band along gumlines.
Abrasion/wear/erosion: glossy, firm surfaces; erosion thins enamel and looks yellow.
Tartar (calculus): hard deposits; rough to the touch but not softened tooth.
Safe at-home self-check
Setup: Bright light + mirror; don’t pick with metal objects.
Check four things:
Color (chalky white, brown/black)
Surface (matte vs. glossy; soft/rough vs. hard)
Food trapping (persistent)
Sensitivity (sweet/cold/biting)
Red flags: Spots lasting >2 weeks despite excellent cleaning; obvious softness or breaking edges; ongoing trapping/halitosis/bite pain; spontaneous or night pain.
What to do at each stage (quick table)
Early white spot — Home: fluoride toothpaste 2×/day; cut sugar frequency; meticulous cleaning. Office: fluoride varnish; resin infiltration; monitor.
Softened, no hole — Home: book a visit soon. Office: micro-invasive cleaning + composite restoration.
Cavitated — Home: keep clean; avoid hard/sticky foods. Office: filling/inlay/onlay; deep lesions may need pulp cap or root canal.
Root caries — Home: soft-bristle/electric brush; interdental brushes. Office: remove decay + restore; root-surface prevention plan.
Prevention you can see
Visible plaque at gumlines, inflamed red gums, very deep grooves, and routine food trapping signal higher risk for tooth decay.
Routine: 2 minutes × 2/day brushing + daily floss/interdental brush. Sugar frequency matters more than total amount. Orthodontic patients benefit from a water flosser around brackets/wires.
Smart sugar strategy (what really matters)
Every “snack event” feeds cavity-causing bacteria for 20–30 minutes. Five small sugary hits across the day are riskier than the same sugar eaten once with a meal. Pair sweets with main meals, sip water after, and avoid grazing between meals—this reduces the acid time that drives tooth decay. For sports or flavored drinks, limit to short windows and rinse with plain water; don’t brush immediately after acidic beverages—wait 20–30 minutes so enamel can re-harden.
Tools & daily habits to lower risk
Fluoride toothpaste: Adults 1000–1500 ppm; kids: smear (<3) / pea-size (3–6). Spit; no heavy rinsing.
Brush choice: Soft bristles; an electric toothbrush improves plaque removal and consistency.
Between teeth: Floss nightly; use interdental brushes if spaces allow; a water flosser is a helpful adjunct.
Parents: For toddlers, wipe gums/teeth after the last feed; schedule a first dental visit by age one; ask about sealants on erupting molars.
Photo tips for your next checkup (adds real value)
If you can’t be seen immediately, good photos help triage: dry the tooth, use a steady light, shoot straight on and at a slight angle.
When to see a dentist
Persistent white or dark areas, food trapping, sensitivity, a visible pit or hole, swelling, or any spontaneous/night pain—book an exam. Early fixes are smaller, cheaper, and preserve more natural tooth.
Medical note
This article provides general oral-health education and does not replace diagnosis or treatment. If you suspect tooth decay, please see a dentist for personalized care.




